"Psoriasis" is derived from the Greek word "psora", meaning: I scratch. In Germany, most people use the word "Schuppenflechte" because silvery-white scales ("Schuppen") cover the body like a lichen ("Flechte"). But this term is misleading because psoriasis is not just a skin disease. It is a complex inflammatory disease that affects the entire body. In the English-speaking world, therefore, the term "psoriatic disease" is increasingly being used.
Therapy of Psoriasis Vulgaris
"Psoriasis" is derived from the Greek word "psora". This means: I scratch.
In Germany, most people use the word "psoriasis" because silvery-white scales cover the body like a lichen. But this term is misleading because psoriasis is not just a skin disease. It is a complex inflammatory disease that affects the entire body. In English-speaking countries, the term "psoriatic disease" is therefore increasingly being used.
Physicians base their decisions on so-called guidelines.
These are treatment recommendations based on the latest scientific findings.
In 2006, the first S3 guideline "Therapy of psoriasis vulgaris" was published by the German Dermatological Society (DDG) and the Professional Association of German Dermatologists (BVDD) with the participation of members of the German Psoriasis Association (DPB). S3 designates the highest quality level of the development methodology of a guideline. It includes worldwide knowledge verified by studies (evidence-based) in the evaluation of the therapies described.
In order to share this knowledge with patients, the DPB published a version for patients - the DPB patient guideline - immediately after the publication of the first S3 guideline "Therapy of psoriasis vulgaris". In this guideline, the contents of the S3 guideline were presented in an easily understandable way for patients and supplemented with additional information to serve the understanding of the disease and its treatment. Since 2006, the DPB has made a total of three revisions to its DPB patient guideline in line with the updates made to the S3 guideline. The latest revision took place after release of the new S3 guideline in summer 2025.

The basis for the creation of this "Therapy guideline psoriasis. A guide for patients" is the S3 guideline "Therapy of psoriasis vulgaris", which was published in an updated version in 2022.
It is not legally binding, but it helps to improve treatment for everyone with psoriasis.
Click on “Find out more” to learn about the guideline for the treatment of psoriasis.
Therapy of Psoriasis Vulgaris
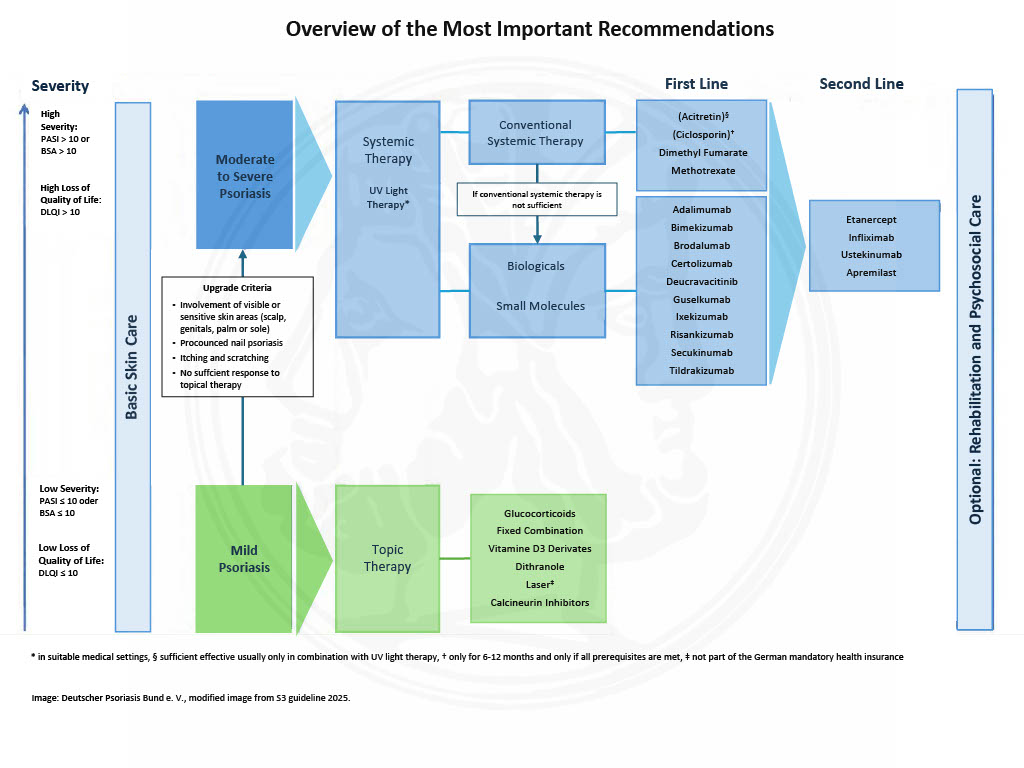
If only a few areas of the body with a small surface area are affected, external (topical) therapies with active ingredients in creams, ointments, solutions or foams are primarily used according to the S3 guideline. With increasing extent or insufficient results, this therapy is occasionally combined with UV light therapy (treatment with ultraviolet light). If the psoriasis is extensive or if external therapies do not respond sufficiently, internal (systemic) therapy with tablets or injections is usually carried out. This can also be combined with external therapy. If a combination of therapies is especially important, this is mentioned in particular in this guideline.
In addition to active ingredient therapy for psoriasis, the skin usually requires basic therapy without active ingredients. This should be the basis for any further treatment. For this purpose, moisturizing and nourishing creams, ointments or lotions are used. Their use improves the condition of the skin and helps to prolong the symptom-free period.
How can you distinguish between mild and severe psoriasis?
To assess the severity of the disease, both the skin symptoms and the quality of life are taken into account. Various scales are used to measure this, which we will present below.
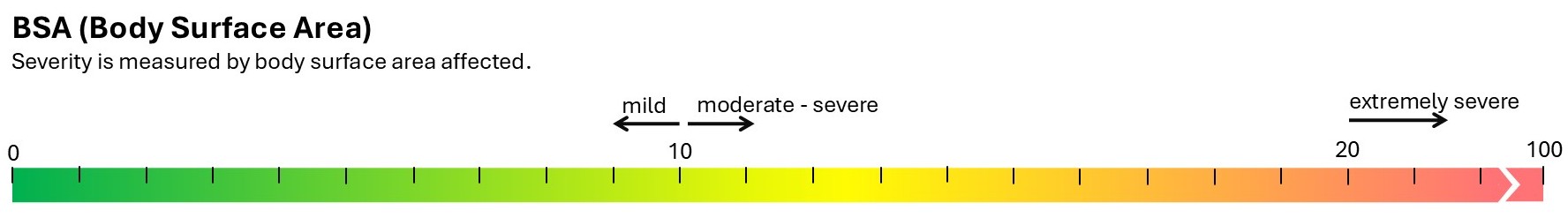
BSA
BSA stands for body surface area and indicates the extent of the affected skin area. The affected area is usually expressed as a percentage of the total skin area. For simplicity, an approximate percentage is assigned to each individual body region:
- Head 9%
- Right arm 9%
- Left arm 9%
- Front torso 18%
- Back torso 18%
- Genital area 1%
- Right leg 18%
- Left leg 18%
A BSA value of 10 or lower is considered mild psoriasis, above 10 is moderate to severe psoriasis. Above 20, psoriasis is considered particularly severe.
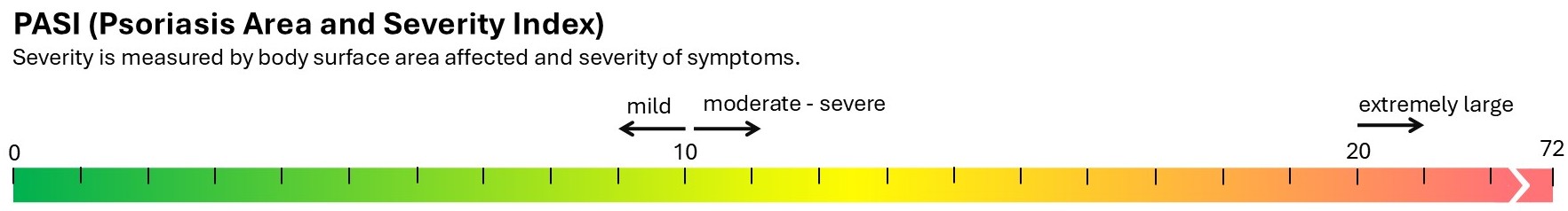
PASI
PASI stands for Psoriasis Area and Severity Index and indicates the extent of the affected skin area and the severity of the symptoms. The affected skin area is determined as a percentage, as with BSA. To determine the severity of the symptoms, the degree of redness, scaling, and thickness of the skin plaques are considered. A score of 0-4 points is assigned for each of these factors, with 0 points indicating no symptoms and 4 points indicating very severe symptoms. Finally, the value for the affected skin area and the points for the severity of the symptoms are combined to determine a final score, which can range from 0 to 72.
A PASI score of 10 or lower indicates mild psoriasis, while a score above 10 indicates moderate to severe psoriasis. A score of 20 or higher is considered particularly severe psoriasis. These thresholds are the same for BSA and PASI scores.
Nowadays, doctors use the PASI score more often than the BSA score.
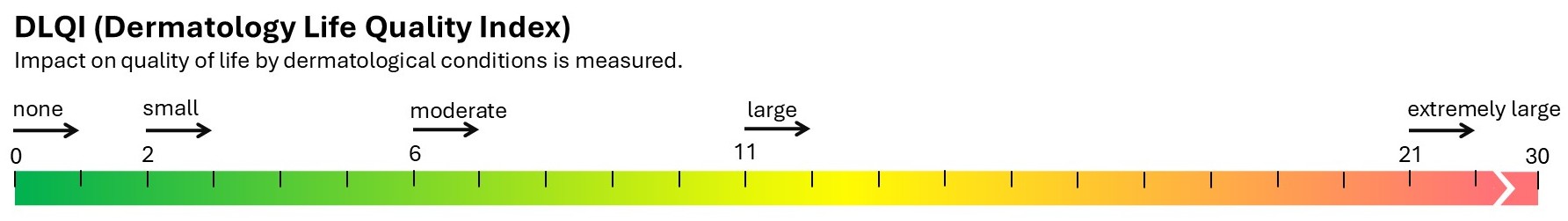
DLQI
DLQI stands for Dermatology Life Quality Index and indicates the degree to which your dermatological condition affects your quality of life. To determine your DLQI score, you will be asked to complete a questionnaire consisting of 10 questions that assess the impact of your condition on your everyday life, work or school, leisure activities, clothing, and personal relationships. The DLQI can range from 0 to 30, and the higher the score, the greater the impact on your quality of life.
Determine the severity using PASI/BSA and DLQI
Ideally, both skin symptoms and impairment of quality of life should be taken into account when determining the severity.
The following classification has been agreed upon:
Mild psoriasis:
BSA ≤10 or PASI ≤10
DLQI ≤10
Moderate to severe psoriasis:
BSA >10 or PASI >10
DLQI >10
Severe psoriasis:
PASI ≥20
DLQI ≥15
as well as in cases of rapid deterioration of findings, severe involvement of the hands and/or feet,
the scalp, the face, the nails, or the genital area.
What does PASI75 mean?
The term PASI75 is used to express how well a therapy is working. This is because the improvement in symptoms, measured as a PASI score, is used to determine whether a therapy is successful. Currently, the goal is to achieve a 75% improvement in the PASI score, which is abbreviated as “PASI 75.”
S3 guideline as download
The current S3 guideline "Treatment of Psoriasis Vulgaris" is also available on the website of the Deutscher Psoriasis Bund e. V. (DPB).
External therapy, often applied in the form of creams and ointments, plays a crucial role in the treatment of many skin conditions. Here, specific active substances are applied to targeted areas of the skin to effectively relieve from symptoms and promote skin health.
Internal (=systemic) medications are used in cases of greater extent of psoriasis, severely inflammated areas and high loss of quality of life.
Internal (also known as systemic) medication is used for moderate to severe psoriasis, especially if the skin is affected over a large area, there are severely inflamed areas or the quality of life is significantly impaired.
Active Substances of Internal Therapy
Internal (also known as systemic) medication is used for moderate to severe psoriasis, especially if the skin is affected over a large area, there are severely inflamed areas or the quality of life is significantly impaired.
They may also be necessary in cases of pronounced infestation of the hairy head, visible areas (e.g. face, back of the hand) or in the genital area - often associated with severe itching - as well as in cases of severe nail changes on at least two fingernails - the so-called upgrade criteria. Deviations from these general guideline values are permitted in individual cases if medically necessary and appropriate.
The active substances currently available for systemic therapy are shown on the main page.
They are usually divided into conventional drugs and biologicals. The conventional drugs are also referred to as non-biologicals.
The approval status plays a particularly important role for prescription. Drugs with a "firstline" approval should be prescribed first, with non-biologics being given preference over biologicals for economic reasons, as their annual therapy costs are significantly lower. This "economic efficiency requirement" is found in §12 of the German Social Code Book V. If at least one conventional (non-biological) drug was not tolerated, was not effective, or was not allowed to be used, for example, due to medical reasons, a biologic can be prescribed. If it is foreseeable that the non-biologics do not offer sufficient prospect of treatment success, then a biological can also be started straight away. This is often the case with extremely high severity.
Of the biologicals, those with an approval as a "first-line" preparation are used first, with further changes also involving a drug with a "second-line" approval.
In any case, in Germany, psoriasis offers the possibility of an individual choice of therapy from a wide range of approved systemic medications.
Control Examinations
Medications administered internally (systemic) can cause side effects. To detect these at an early stage, doctors conduct regular check-ups on patients receiving systemic treatment. Before starting systemic therapy, doctors also carefully check whether the drug is suitable in the individual case. The physician determines which laboratory tests or other measures (e.g., measurement of blood pressure) must be conducted for the respective drug in accordance with the recommendations of the specialist information and the guideline.
Patients should always keep the appointments for check-ups made with the doctor.

Retinoids
Derivatives of vitamin A, so-called retinoids (active substance: acitretin), have been used for a very long time as capsules as first-line treatment of psoriasis. The dosage is adjusted to the body weight (usually 0.3 to 0.8 milligrams per kilogram of body weight daily). The effect sets in after four to eight weeks. However, only a small proportion of patients achieve general freedom from symptoms.
Retinoids must not be used in case of kidney or liver damage and in women of childbearing potential. Retinoids always harm the the embryo. Dry lips, dry skin, nosebleeds and temporary hair loss may occur during treatment. As a stand-alone treatment, retinoids are usually not sufficiently effective. Therefore, this agent is often combined with UV light therapy. Women of childbearing potential must ensure safe prevention of pregnancy (protection against conception) for up to three years after treatment with retinoids has stopped.
In view of many more effective and tolerable drugs, retinoids are now only used in exceptional cases in psoriasis vulgaris.
Apremilast
Apremilast is an active substance used in second-line therapy for moderate to severe plaque psoriasis and psoriatic arthritis. After a short phase of dose escalation to improve tolerability, apremilast is taken twice daily as 30 mg tablets in maintenance therapy. The effect is delayed; after eight to twelve weeks, it can be assessed whether sufficient healing has occurred. A small proportion of patients achieve a largely symptom-free state.
Apart from occasional gastrointestinal complaints, tolerability is good. Apremilast is also a relatively safe drug, with few adverse events occurring in all studies. It is also approved for psoriatic arthritis, so this form of psoriasis may also be a reason for treatment with apremilast.
Ciclosporin
The active ingredient ciclosporin has been approved for first-line treatment of psoriasis since 1993. Capsules or an oral solution are taken daily in a dosage adjusted to body weight (2.5 to 5 milligrams per kilogram of body weight). The effect can be expected after approximately four weeks. Most patients achieve a high degree of remission.
Ciclosporin must not be used in case of kidney dysfunction, uncontrollable high blood pressure or malignant cancer. Side effects may include kidney and liver dysfunction, increased blood pressure and gastrointestinal complaints. Interactions may occur when taking other medications. Patients who have previously undergone prolonged UV light therapy should not use ciclosporin. They have an increased risk of developing skin cancer.
Given that there are many medications that are more suitable for long-term therapy, ciclosporin is now only used in exceptional cases for psoriasis vulgaris.
Deucravacitinib
Since 2022, deucravacitinib has been approved for the treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy. It is taken orally as a tablet once daily (dose: 6 milligrams). Improvement can often be seen within a few weeks. Many patients achieve a clear reduction of skin symptoms.
Tyrosine kinase 2 (TYK2) inhibitor
Deucravacitinib selectively blocks the enzyme tyrosine kinase 2, which plays a key role in the signaling of pro-inflammatory messengers such as interleukin-23, interleukin-12, and type I interferons. Unlike traditional JAK inhibitors, deucravacitinib binds to the regulatory domain of TYK2, which may result in a more favorable side effect profile. However, possible side effects include upper respiratory tract infections, headaches, and nausea. Serious infections are rare but possible, so medical monitoring remains important. Before starting therapy, infections—especially tuberculosis—should be ruled out.
Dimethyl Fumarate
Dimethyl fumarate is a fumaric acid ester, which have been widely used as a first-line medication for the internal treatment of psoriasis since 1994. The tablets are usually taken according to a prescribed schedule. The dose can be adjusted individually. The effect of the treatment can be expected after approximately six weeks. For many patients, the therapy can lead to a significant reduction in symptoms. Dimethyl Fumarate must not be taken in case of gastrointestinal or kidney disease. The therapy may cause gastrointestinal complaints, sudden reddening of the skin and changes in the blood count.
Fumaric Acid Ester
Fumaric acid ester (Fumaderm®) will no longer be manufactured after 2025. The last remaining stocks are probably only available in the first few months of 2025 – please speak to your doctor soon about approved alternatives.
Methotrexate
One of the longest-used drugs for the first-line treatment of psoriasis is the active substance methotrexate (MTX). It is injected into the skin once a week or taken as a tablet. The injection is more effective and is usually better tolerated. The dosage is determined individually and is usually between 15 and 25 milligrams per week. The effect sets in after approximately four to eight weeks. In many patients, the therapy can lead to a mostly disappearance of symptoms. Methotrexate must not be given to patients with impaired liver function. The treatment can cause liver damage, pneumonia, destruction of bone marrow and damage to the kidneys. Patients should avoid alcohol during treatment with methotrexate.
Adalimumab
Since 2005, adalimumab has been approved for the treatment of psoriatic arthritis and, later, as a first-line treatment for moderate to severe plaque psoriasis. It is administered by injection into the skin every two weeks (dosage: 40 milligrams). The effect sets in after four to eight weeks. A large proportion of patients achieve a high degree of remission. If the effect is insufficient, treatment with 40 milligrams of adalimumab once a week can be continued for up to three months.
TNF-Alpha inhibitors
This group of biologicals blocks the pro-inflammatory messenger substance called tumour necrosis factor alpha. It is also known as a TNF-Alpha inhibitor. Biologicals of the TNF-Alpha inhibitor type must not be used in case of severe heart disease (heart failure). Severe infections can also occur during therapy with TNF-Alpha inhibitors. All infections occurring during therapy therefore require immediate medical attention. Before starting therapy, tuberculosis, liver inflammation and HIV infection must always be ruled out with certainty.
Bimekizumab
This molecule is a relatively new active substance for first-line treatment of moderate to severe plaque psoriasis and was approved for adults in 2021. The active substance blocks the messenger substances IL-17A and IL-17F. The effect sets in within the first two weeks. The recommended dose is 320 milligrams, administered in two injections under the skin (subcutaneously) every four weeks until week 16 and then every eight weeks thereafter. In some patients weighing more than 120 kilograms who did not achieve complete clearance of their skin by week 16, bimekizumab at a dose of 320 milligrams every four weeks after week 16 may further improve the response to treatment.
Interleukin-17 inhibitors
Active substances in this group of biologicals block the pro-inflammatory messenger substance interleukin-17 (IL-17) or its binding site (receptor). There are currently four blockers available. They are all approved as first-line therapies for moderate to severe plaque psoriasis. They are very effective. Two active substances (ixekizumab, secukinumab) are also approved for psoriatic arthritis. A notable side effect of this group is the frequent occurrence of localised yeast infections in the mouth or throat and, more rarely, in the genital area or body folds. Pre-existing chronic intestinal inflammation may also worsen. With all IL-17 inhibitors, the majority of patients achieve a high degree of remission and respond quite quickly within a few weeks.
Brodalumab
The active substance has been approved for first-line treatment of moderate to severe plaque psoriasis in adults since 2017. The active substance blocks the receptor on cells to which IL-17A binds, as well as other members of the interleukin-17 family. The effect sets in within the first two weeks. The dosage is 210 milligrams at the start, after one and two weeks, then 210 milligrams every two weeks in maintenance therapy.
Interleukin-17 inhibitors
Active substances in this group of biologicals block the pro-inflammatory messenger substance interleukin-17 (IL-17) or its binding site (receptor). There are currently four blockers available. They are all approved as first-line therapies for moderate to severe plaque psoriasis. They are very effective. Two active substances (ixekizumab, secukinumab) are also approved for psoriatic arthritis. A notable side effect of this group is the frequent occurrence of localised yeast infections in the mouth or throat and, more rarely, in the genital area or body folds. Pre-existing chronic intestinal inflammation may also worsen. With all IL-17 inhibitors, the majority of patients achieve a high degree of remission and respond quite quickly within a few weeks.
Certolizumab
This active substance differs from other biologicals in its chemical structure. It has first-line approval for moderate to severe psoriasis vulgaris (plaque psoriasis) and second-line approval for psoriatic arthritis. A large proportion of patients achieve a high degree of remission. The recommended starting dose for adult patients is 400 mg (administered in two subcutaneous injections of 200 mg each) in weeks 0, 2, and 4. In cases of psoriatic arthritis, MTX should continue to be administered during treatment as far as possible. A maintenance dose of 200 mg every two weeks is recommended. If there is a clinical response, an alternative maintenance dose of 400 mg every 4 weeks may be considered. One advantage of certolizumab pegol is that it cannot pass through the placenta to the child in pregnant women.
TNF-Alpha inhibitors
This group of biologicals blocks the pro-inflammatory messenger substance called tumour necrosis factor alpha. It is also known as a TNF-Alpha inhibitor. Biologicals of the TNF-Alpha inhibitor type must not be used in case of severe heart disease (heart failure). Severe infections can also occur during therapy with TNF-Alpha inhibitors. All infections occurring during therapy therefore require immediate medical attention. Before starting therapy, tuberculosis, liver inflammation and HIV infection must always be ruled out with certainty.
Etanercept
Etanercept has been approved since 2002 as a second-line treatment for psoriatic arthritis and since 2004 as a second-line treatment for moderate to severe plaque psoriasis. The usual dosage today is 50 milligrams once a week. The onset of action can be expected after four to eight weeks. Since a significantly smaller proportion of patients achieve extensive remission than with other biologicals, etanercept is now rarely used for new patients.
It has now also been approved for children and adolescents aged six years and older.
TNF-Alpha inhibitors
This group of biologicals blocks the pro-inflammatory messenger substance called tumour necrosis factor alpha. It is also known as a TNF-Alpha inhibitor. Biologicals of the TNF-Alpha inhibitor type must not be used in case of severe heart disease (heart failure). Severe infections can also occur during therapy with TNF-Alpha inhibitors. All infections occurring during therapy therefore require immediate medical attention. Before starting therapy, tuberculosis, liver inflammation and HIV infection must always be ruled out with certainty.
Golimumab
The active substance is currently only approved for second-line treatment of psoriatic arthritis and has only moderate efficacy on the skin. The dose is 50 milligrams every four weeks. For patients weighing over 100 kilograms and with an insufficient response, the dose can be increased to 100 milligrams every four weeks.
Guselkumab
Guselkumab has been approved as a first-line treatment for moderate to severe plaque psoriasis in adults since the end of 2017. The effect sets in within the first two weeks. The initial dosage is 100 milligrams at the start and after four weeks. It is then administered every eight weeks as maintenance therapy. The majority of patients achieve a high degree of remission. It has now also been approved for psoriatic arthritis.
Interleukin-23 inhibitors
The first active substance in this group, ustekinumab, blocked not only the messenger substance IL-23, but also IL-12 by binding to a common subunit of the molecules (p40).
Subsequently, the molecules guselkumab, risankizumab and tildrakizumab were developed, which only block IL-23 (p19 subunit) but are even more effective. A special feature of all these molecules is that they only need to be administered every two to three months during the maintenance phase.
Infliximab
Infliximab has been approved for the treatment of moderate to severe plaque psoriasis since 2005. It is administered by infusion in a doctor's office and is given every eight weeks as maintenance therapy. Dosage: Five milligrams per kilogram of body weight. The effect sets in after one to two weeks. Infusion reactions may occur during therapy. Infliximab is a fast-acting substance for the treatment of plaque psoriasis.
A large proportion of patients achieve a high degree of remission, but the effect tends to weaken over the course of treatment more frequently than with other medications. Low-dose methotrexate (five to 10 milligrams per week) is often given in addition to infliximab therapy.
TNF-Alpha inhibitors
This group of biologicals blocks the pro-inflammatory messenger substance called tumour necrosis factor alpha. It is also known as a TNF-Alpha inhibitor. Biologicals of the TNF-Alpha inhibitor type must not be used in case of severe heart disease (heart failure). Severe infections can also occur during therapy with TNF-Alpha inhibitors. All infections occurring during therapy therefore require immediate medical attention. Before starting therapy, tuberculosis, liver inflammation and HIV infection must always be ruled out with certainty.
Ixekizumab
The active substance has been approved 2016 for first-line treatment of moderate to severe plaque psoriasis and is now also approved for psoriatic arthritis. The effect sets in within the first two weeks. Initially, 80 milligrams are administered every two weeks for three months, followed by 80 milligrams every four weeks as maintenance therapy. It is now also approved for children and adolescents aged six years and older. The undesirable effects of the drug have been investigated in numerous studies, . Possible side effects include reactions at the injection site, upper respiratory tract infections, pain in the oropharynx area, nausea, fungal infections, and mucocutaneous herpes simplex.
Interleukin-17 inhibitors
Active substances in this group of biologicals block the pro-inflammatory messenger substance interleukin-17 (IL-17) or its binding site (receptor). There are currently four blockers available. They are all approved as first-line therapies for moderate to severe plaque psoriasis. They are very effective. Two active substances (ixekizumab, secukinumab) are also approved for psoriatic arthritis. A notable side effect of this group is the frequent occurrence of localised yeast infections in the mouth or throat and, more rarely, in the genital area or body folds. Pre-existing chronic intestinal inflammation may also worsen. With all IL-17 inhibitors, the majority of patients achieve a high degree of remission and respond quite quickly within a few weeks.
Risankizumab
Risankizumab is approved for the treatment of moderate to severe plaque psoriasis as a first-line therapy in adults since 2019. The effect sets in within four weeks. The initial dosage is 150 milligrams at the start and after four weeks. It is then administered every twelve weeks as maintenance therapy. The majority of patients achieve a high degree of remission. It has now also been approved for psoriatic arthritis.
Interleukin-23 inhibitors
The first active substance in this group, ustekinumab, blocked not only the messenger substance IL-23, but also IL-12 by binding to a common subunit of the molecules (p40).
Subsequently, the molecules guselkumab, risankizumab and tildrakizumab were developed, which only block IL-23 (p19 subunit) but are even more effective. A special feature of all these molecules is that they only need to be administered every two to three months during the maintenance phase.
Secukinumab
Secukinumab was the first IL-17A inhibitor and has been approved 2015 for the treatment of moderate to severe plaque psoriasis as first-line therapy. The effect sets in within the first four weeks. For therapy, 300 milligrams are given once a week for four weeks, then 300 milligrams monthly in maintenance therapy. If the effect weakens, the 300 milligrams can also be given every two weeks for a while. For psoriatic arthritis, the starting and maintenance dose is 150 milligrams. The injection intervals are the same as for plaque psoriasis. It is also approved for kids and teens aged six and older.
Interleukin-17 inhibitors
Active substances in this group of biologicals block the pro-inflammatory messenger substance interleukin-17 (IL-17) or its binding site (receptor). There are currently four blockers available. They are all approved as first-line therapies for moderate to severe plaque psoriasis. They are very effective. Two active substances (ixekizumab, secukinumab) are also approved for psoriatic arthritis. A notable side effect of this group is the frequent occurrence of localised yeast infections in the mouth or throat and, more rarely, in the genital area or body folds. Pre-existing chronic intestinal inflammation may also worsen. With all IL-17 inhibitors, the majority of patients achieve a high degree of remission and respond quite quickly within a few weeks.
Tildrakizumab
Tildrakizumab has been approved 2018 for the treatment of moderate to severe plaque psoriasis as first-line therapy in adults. The effect sets in within the first four to six weeks. The initial dosage is 100 milligrams at the start and after four weeks. It is then administered every twelve weeks as maintenance therapy. In very severe cases, 200 milligrams may also be given. The majority of patients achieve a high degree of remission.
Interleukin-23 inhibitors
The first active substance in this group, ustekinumab, blocked not only the messenger substance IL-23, but also IL-12 by binding to a common subunit of the molecules (p40).
Subsequently, the molecules guselkumab, risankizumab and tildrakizumab were developed, which only block IL-23 (p19 subunit) but are even more effective. A special feature of all these molecules is that they only need to be administered every two to three months during the maintenance phase.
Ustekinumab
The active substance ustekinumab has been approved as a second-line medication in 2009. It is injected into the skin twice in a 4-weeks-interval, and afterwards every twelve weeeks. Dosage: 45 milligrams per injection for patients weighing up to 100 kilograms and 90 milligrams for patients weighing more than 100 kilograms. The effect sets in after six to twelve weeks, and a large proportion of patients achieve a high degree of remission. It is also approved for psoriasis vulgaris in children and adolescents aged six years and older, as well as for psoriatic arthritis in adults.
UV light therapy has been a proven therapeutic approach for a long time but is now increasingly rarely performed. As with internal medications, the use of light therapy also depends on the severity of the skin changes and the restrictions on quality of life.
Basic Therapy
Basic therapy is the moisturizing and caring treatment of the skin with ointments, creams and lotions that are free of (medical) active substances. The choice of the appropriate preparation depends on the condition of the skin, on how dry and/or how inflamed the skin is. Depending on the desired purpose, the skin care product may contain three to ten percent urea. Urea binds moisture in the upper layers of the skin.
Basic therapeutic care is a particularly important part of the complementary treatment of psoriasis. This applies equally to the complementary therapy of acute psoriasis foci and to the follow-up treatment of healing skin. Basic therapy can help restore an intact skin barrier. However, basic therapy is usually not sufficient as the sole treatment for psoriasis. Basic therapy can be combined with all forms of therapy for psoriasis.
Basic Therapy
Basic therapy is the moisturizing and caring treatment of the skin with ointments, creams and lotions that are free of (medical) active substances. The choice of the appropriate preparation depends on the condition of the skin, on how dry and/or how inflamed the skin is. Depending on the desired purpose, the skin care product may contain three to ten percent urea. Urea binds moisture in the upper layers of the skin.
Basic therapeutic care is a particularly important part of the complementary treatment of psoriasis. This applies equally to the complementary therapy of acute psoriasis foci and to the follow-up treatment of healing skin. Basic therapy can help restore an intact skin barrier. However, basic therapy is usually not sufficient as the sole treatment for psoriasis. Basic therapy can be combined with all forms of therapy for psoriasis.
Psychosomatic Treatment and Training
Psoriasis is often accompanied by considerable suffering and psychological stress. Conversely, many patients with psoriasis state that their psoriasis worsens under stress and psychological strain or that new foci even appear. In these cases, it makes sense to clarify not only the condition of the skin, but also psychosomatic interactions as part of the diagnosis. In some patients with psoriasis, in addition to treatment of the psoriatic skin, psychological or psychotherapeutic treatment may also be helpful, especially in cases of high psychological distress.
Training courses for patients have also proved very helpful. Such training sessions provide information on psoriasis and practical advice on therapies, skin care and ways to reduce stress.
Better management of one's own psoriasis is an important goal of these training courses. Special training courses are routinely conducted during inpatient rehabilitation but are only offered in the outpatient area in individual centers. The costs for outpatient training are not generally covered by statutory health insurance.
Psychosomatic Treatment and Training
Psoriasis is often accompanied by considerable suffering and psychological stress. Conversely, many patients with psoriasis state that their psoriasis worsens under stress and psychological strain or that new foci even appear. In these cases, it makes sense to clarify not only the condition of the skin, but also psychosomatic interactions as part of the diagnosis. In some patients with psoriasis, in addition to treatment of the psoriatic skin, psychological or psychotherapeutic treatment may also be helpful, especially in cases of high psychological distress.
Training courses for patients have also proved very helpful. Such training sessions provide information on psoriasis and practical advice on therapies, skin care and ways to reduce stress.
Better management of one's own psoriasis is an important goal of these training courses. Special training courses are routinely conducted during inpatient rehabilitation but are only offered in the outpatient area in individual centers. The costs for outpatient training are not generally covered by statutory health insurance.
Special Localizations of Psoriasis Vulgaris
In psoriasis vulgaris, areas with special disease value may be affected, which are not addressed separately in the guideline. These are mainly the scalp, the nails, the face, but also the anal and genital areas. They are of particular importance because they are often associated with a special degree of suffering, although their area is not very large, and they are not adequately covered by the PASI area score. Therefore, their severity must be assessed separately. Also, severe infestation of these areas alone is a criterion for internal therapy (system therapy), since external (topical) therapy often does not have sufficient effect or sometimes there is a contraindication to certain topical drugs in a body region. However, psoriasis lesions in these areas do respond well to system therapy.
Psoriasis in the Body Folds (intertriginous psoriasis)
The skin in body folds can also develop psoriasis. Most affected are armpits, folds in the groin area (inguinal folds), the skin under the female breast, on the navel and in the anal fold (butt fold). In overweight patients, psoriasis may also develop in abdominal folds. In body folds, skin lies on skin. The skin there is always moist. This makes it easy for the scales to peel off. Usually only a bright red, shiny focal point is still visible.
In the absence of the characteristic scales, diagnosis is sometimes difficult. There may be confusion with fungal infections and eczema. For treatment, corticosteroids are used in the short term in a base as milk/lotion, in cream or paste. Subsequently, the wrinkles should be kept dry by care to prevent recurrence of psoriasis there. A trial with vitamin D-like preparations (emulsion, cream, foam) is possible, although they are less effective and may cause irritation.

Psoriasis of the Scalp (psoriasis capitis)
In more than 70 percent of patients with psoriasis, foci are also present on the hairy head, at least temporarily. They can be localized or extensive and typically extend beyond the hairline. The foci are strongly scaling and inflammatory reddened. Psoriasis of the scalp may occasionally be accompanied by hair loss, which usually resolves after successful treatment. Itching is almost always present.
The goal of treatment is to restore a scalp free of scaling, redness and itching. This is most effectively done by solutions with corticoids (some contain alcohol, which can burn) or foams. Corticoids are particularly effective for itching. On the scalp, they are well tolerated even with prolonged use and do not produce relevant side effects. For longer-term use, supplementary preparations with vitamin D3 derivatives are suitable, also in fixed combination with a corticosteroid. If there is a tendency to recurrences, proactive treatment has proven effective, in which corticosteroid is used only once or twice a week.
Patients report good experiences with UV light combs. However, before using them, the dandruff must be removed. This treatment is also very time-consuming.
The basis for this is the use of shampoos with dandruff-relieving effect, which are also available in drug stores. Ingredients can be, for example: Zinc pyrithione or ciclopirox. In case of strong, stuck dandruff, a pre-treatment with wash-out emulsifying creams or solutions with salicylic acid or spreading oils can be applied. However, active ingredient therapy is more important, since desquamative treatment alone does not reduce the formation of new scales.

Psoriasis of the Nails
In up to 69 percent of patients with psoriasis, the finger and/or toenails are conspicuously changed. Even more frequent is a disease of the nails with simultaneous psoriatic arthritis. About 80 percent of patients with psoriatic arthritis also have changes in their nails. As a rule, several nails on hands and feet are diseased on both sides at the same time. There are different changes on the nails. In decreasing frequency, the most important ones are described.
Spotted Nails
Spotted nails are quite common. Spots are small to pinhead sized dimples (depressions) in the nail plate. The number, size and depth of the spots can vary. Spots are usually randomly distributed but may also be arranged along longitudinal lines. Fingernails are always more frequently affected than toenails.

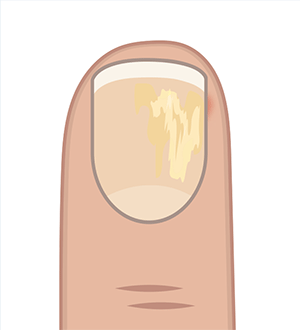
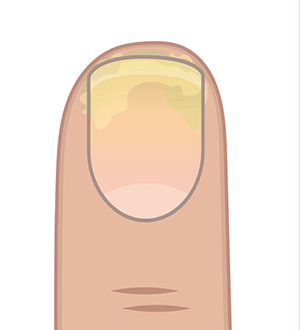
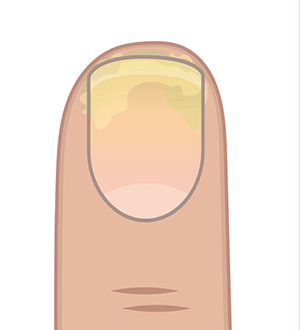
Psoriatic Oil Spots, Detachment of the Nail Plate (distal onycholysis)
The nail bed and the skin under the front part of the nail are involved. Yellow-greyish, oval discolorations are seen. They come from the inflammation with scaling under the nail plate in the nail bed. In case of pronounced changes, the nail plate may detach from the nail bed.
Severe Scaling under the Nail (subungual hyperkeratosis)
Very severe scaling may occur under the nail. If the area where the nail grows out of the nail bed is also diseased, the nail plate may lift off there.

Crumb Nails (onychodystrophy)
In a crumb nail, the nail plate is destroyed. The nail itself is crumbly and distended.
Treatment of Nails
In the treatment of psoriasis of the nails, the success of the therapy only becomes apparent after a long-time delay, as the nails only grow back very slowly. A fingernail needs about six months, a toenail up to twelve months for complete renewal. Spotted nails and oil stains are sometimes not treated; if necessary, they can be covered with nail polish. For milder forms of psoriasis of the nails with detachment of the nail plate or changes in the nail substance, corticosteroids in solutions or a vitamin D3 derivative in combination with a corticosteroid in ointment, gel, solution or foam are applied.
The treatment lasts several months. In individual cases, injections with corticosteroid crystal solutions can be successful. These are gladly injected needle-free with a "Dermojet", which is less painful.
In more severe cases or if external measures fail, nail psoriasis is treated with internal medications. In principle, (almost) all drugs approved for psoriasis are suitable. However, the prospect of a response is higher with the stronger-acting system therapeutics. Biologics are therefore particularly suitable for the treatment of psoriasis of the nails.
Special Localizations of Psoriasis Vulgaris
In psoriasis vulgaris, areas with special disease value may be affected, which are not addressed separately in the guideline. These are mainly the scalp, the nails, the face, but also the anal and genital areas. They are of particular importance because they are often associated with a special degree of suffering, although their area is not very large, and they are not adequately covered by the PASI area score. Therefore, their severity must be assessed separately. Also, severe infestation of these areas alone is a criterion for internal therapy (system therapy), since external (topical) therapy often does not have sufficient effect or sometimes there is a contraindication to certain topical drugs in a body region. However, psoriasis lesions in these areas do respond well to system therapy.
Psoriasis in the Body Folds (intertriginous psoriasis)
The skin in body folds can also develop psoriasis. Most affected are armpits, folds in the groin area (inguinal folds), the skin under the female breast, on the navel and in the anal fold (butt fold). In overweight patients, psoriasis may also develop in abdominal folds. In body folds, skin lies on skin. The skin there is always moist. This makes it easy for the scales to peel off. Usually only a bright red, shiny focal point is still visible.
In the absence of the characteristic scales, diagnosis is sometimes difficult. There may be confusion with fungal infections and eczema. For treatment, corticosteroids are used in the short term in a base as milk/lotion, in cream or paste. Subsequently, the wrinkles should be kept dry by care to prevent recurrence of psoriasis there. A trial with vitamin D-like preparations (emulsion, cream, foam) is possible, although they are less effective and may cause irritation.

Psoriasis of the Scalp (psoriasis capitis)
In more than 70 percent of patients with psoriasis, foci are also present on the hairy head, at least temporarily. They can be localized or extensive and typically extend beyond the hairline. The foci are strongly scaling and inflammatory reddened. Psoriasis of the scalp may occasionally be accompanied by hair loss, which usually resolves after successful treatment. Itching is almost always present.
The goal of treatment is to restore a scalp free of scaling, redness and itching. This is most effectively done by solutions with corticoids (some contain alcohol, which can burn) or foams. Corticoids are particularly effective for itching. On the scalp, they are well tolerated even with prolonged use and do not produce relevant side effects. For longer-term use, supplementary preparations with vitamin D3 derivatives are suitable, also in fixed combination with a corticosteroid. If there is a tendency to recurrences, proactive treatment has proven effective, in which corticosteroid is used only once or twice a week.
Patients report good experiences with UV light combs. However, before using them, the dandruff must be removed. This treatment is also very time-consuming.
The basis for this is the use of shampoos with dandruff-relieving effect, which are also available in drug stores. Ingredients can be, for example: Zinc pyrithione or ciclopirox. In case of strong, stuck dandruff, a pre-treatment with wash-out emulsifying creams or solutions with salicylic acid or spreading oils can be applied. However, active ingredient therapy is more important, since desquamative treatment alone does not reduce the formation of new scales.

Psoriasis of the Nails
In up to 69 percent of patients with psoriasis, the finger and/or toenails are conspicuously changed. Even more frequent is a disease of the nails with simultaneous psoriatic arthritis. About 80 percent of patients with psoriatic arthritis also have changes in their nails. As a rule, several nails on hands and feet are diseased on both sides at the same time. There are different changes on the nails. In decreasing frequency, the most important ones are described.
Spotted Nails
Spotted nails are quite common. Spots are small to pinhead sized dimples (depressions) in the nail plate. The number, size and depth of the spots can vary. Spots are usually randomly distributed but may also be arranged along longitudinal lines. Fingernails are always more frequently affected than toenails.

Psoriatic Oil Spots, Detachment of the Nail Plate (distal onycholysis)
The nail bed and the skin under the front part of the nail are involved. Yellow-greyish, oval discolorations are seen. They come from the inflammation with scaling under the nail plate in the nail bed. In case of pronounced changes, the nail plate may detach from the nail bed.
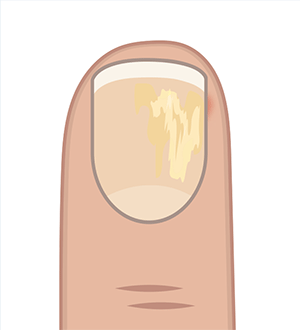
Severe Scaling under the Nail (subungual hyperkeratosis)
Very severe scaling may occur under the nail. If the area where the nail grows out of the nail bed is also diseased, the nail plate may lift off there.

Crumb Nails (onychodystrophy)
In a crumb nail, the nail plate is destroyed. The nail itself is crumbly and distended.
Treatment of Nails
In the treatment of psoriasis of the nails, the success of the therapy only becomes apparent after a long-time delay, as the nails only grow back very slowly. A fingernail needs about six months, a toenail up to twelve months for complete renewal. Spotted nails and oil stains are sometimes not treated; if necessary, they can be covered with nail polish. For milder forms of psoriasis of the nails with detachment of the nail plate or changes in the nail substance, corticosteroids in solutions or a vitamin D3 derivative in combination with a corticosteroid in ointment, gel, solution or foam are applied.
The treatment lasts several months. In individual cases, injections with corticosteroid crystal solutions can be successful. These are gladly injected needle-free with a "Dermojet", which is less painful.
In more severe cases or if external measures fail, nail psoriasis is treated with internal medications. In principle, (almost) all drugs approved for psoriasis are suitable. However, the prospect of a response is higher with the stronger-acting system therapeutics. Biologics are therefore particularly suitable for the treatment of psoriasis of the nails.
Special Forms of Psoriasis
In addition to plaque psoriasis (psoriasis vulgaris), psoriasis can also occur in other manifestations and have different courses. There are special characteristics by which different clinical forms are recognized. The exact determination of the psoriasis is important for the selection of a suitable therapy. These special forms are not part of the S3 guideline but should nevertheless be mentioned here.
Drop-Shaped Psoriasis (guttate psoriasis)
In drop-shaped psoriasis, the foci are up to lentils in size, red and only slightly scaly. Usually, the foci develop very quickly and on the entire skin. More strongly than in all other forms of psoriasis, guttate psoriasis is linked to triggers.
Very often it is preceded by inflammation of the tonsils or scarlet fever (streptococcal infection). Therefore, children and adolescents are often affected by psoriasis guttata. In case of frequent inflammation of the tonsils (tonsillitis), removal of the tonsils in children can improve psoriasis. Triggers can also be medications.
The following agents have been reliably identified as triggers: Lithium, beta-blockers, ACE inhibitors, chloroquine/hydroxychloroquine.
Guttate psoriasis can turn into plaque psoriasis, but it can also heal completely. Topically applied corticosteroids are used in adults often in combination with UVB light therapy and, if necessary, additional treatment of the triggering disease. In children, light therapy should be used with restraint.
Psoriatic Erythroderma
In psoriatic erythroderma, the entire skin is diseased. The skin is completely reddened with inflammation and usually shows a rather fine, loose scaling. Erythroderma is the most severe form of plaque psoriasis and the rarest. There is often severe itching.
Patients feel very ill, have a fever, are fatigued, complain of weight loss and painful joints. The lymph nodes are swollen. Psoriatic erythroderma is usually treated as an inpatient in a skin clinic. Internal medications are always used along with external therapy.
Pustular Psoriasis (psoriasis pustulosa)
In this form, spots (areas) with pustules appear on the skin. The pustules contain mainly white blood cells (neutrophilic granulocytes). While pustules are often caused by infection with bacteria, the contents of psoriatic pustules are sterile. They do not contain bacteria. The pustules are about three millimeters in size and yellowish in color. They burst after some time and dry up, leaving a yellowish crust. Sometimes these pustules appear around foci of plaque psoriasis. The pustules appear very suddenly and especially in the peripheral area of the foci. Often the pustules "grow together" to form a "pustule blanket".
Pustular forms of psoriasis are linked to triggers. It is often preceded by inflammation of the tonsils (streptococcal infection). The use of drugs with active ingredients such as lithium, beta-blockers, ACE inhibitors, chloroquine/hydroxychloroquine are also considered typical triggers. Pustular psoriasis is almost always treated internally. The most important agents are retinoids, methotrexate (MTX) or ciclosporin.
PUVA light therapy may also be useful. Biologics and their biosimilars from the group of tumor necrosis factor antagonists (adalimumab, certolizumab, etanercept, infliximab) as well as the interleukin 17 inhibitors can also be used.
Pustules on the Hands and Feet (pustulosis palmoplantaris (PPP))
Today, this form is no longer attributed to psoriasis; it is considered an independent clinical picture. PPP is restricted exclusively to the palms of the hands and/or soles of the feet. On reddened skin are skin pustules, which in very severe disease can coalesce into small pus lakes. Fresh yellowish pustules and older brown pustules with dried contents and often small annular scaly ruffles are found side by side. If the area is large and there are many fresh yellow pustules, the disease is painful and significantly restricts walking or reaching.
The relapse rate of the disease is remarkably high. It has been scientifically proven that smoking can worsen the course of the disease and increase the relapse rate. Small individual foci can be treated well with externally applied, highly effective corticosteroids. In moderately severe disease, external administration of corticosteroids is supplemented by bath or cream PUVA light therapy. In severe cases, internal medications are given.
Generalized Pustular Psoriasis (GPP)
An independent form of pustular disease is pustular psoriasis distributed over the entire body (generalized pustular psoriasis or pustular psoriasis generalisata). This form, like psoriatic erythroderma, is one of the most severe psoriatic diseases. Many pustules appear very quickly, within hours, on inflammatory reddened skin. The pustules are distributed over a large area of the whole body (generalized). Many patients with generalized pustular psoriasis did not previously have plaque psoriasis as an underlying disease. The general condition of patients with the disease is usually severely impaired, they have a fever and feel fatigued. Treatment must be conducted as an inpatient in a skin clinic. Often, internal measures are also necessary. The therapy is a combination of internal and external medication. External treatment is only supportive, because GPP must usually be treated with internal medication.
In the pustular forms of psoriasis, dithranol should not be used externally and attention must also be paid to the maximum treatable body surface area with the other active ingredients (corticoids, vitamin D3 analogues).
The first drug developed for GPP is spesolimab, which is available for severe cases. Since it is not yet commercially available, it is currently only dispensed through specialized skin clinics.
Paradoxical Psoriasis
With a growing understanding of the underlying inflammation in psoriasis, it is now well established that psoriasis shares some similarity with chronic enteric diseases (CED) and rheumatoid arthritis in the inflammatory mediators involved.
For this reason, patients with rheumatism or IBD are sometimes treated with the same biologics or biosimilars as those with psoriasis. In a few of these treated people with rheumatism or CED, a so-called paradoxical psoriasis occurs in this context. This is called paradoxical because the biologic can also improve psoriasis.
In individual cases, however, the drug used for the treatment of rheumatism can also trigger psoriasis. In this form of psoriasis, the head, hands and feet are often more affected. These areas of the body can be treated well in most cases. If the underlying therapy must be changed, psoriasis usually heals on its own.
Special Forms of Psoriasis
In addition to plaque psoriasis (psoriasis vulgaris), psoriasis can also occur in other manifestations and have different courses. There are special characteristics by which different clinical forms are recognized. The exact determination of the psoriasis is important for the selection of a suitable therapy. These special forms are not part of the S3 guideline but should nevertheless be mentioned here.
Drop-Shaped Psoriasis (guttate psoriasis)
In drop-shaped psoriasis, the foci are up to lentils in size, red and only slightly scaly. Usually, the foci develop very quickly and on the entire skin. More strongly than in all other forms of psoriasis, guttate psoriasis is linked to triggers.
Very often it is preceded by inflammation of the tonsils or scarlet fever (streptococcal infection). Therefore, children and adolescents are often affected by psoriasis guttata. In case of frequent inflammation of the tonsils (tonsillitis), removal of the tonsils in children can improve psoriasis. Triggers can also be medications.
The following agents have been reliably identified as triggers: Lithium, beta-blockers, ACE inhibitors, chloroquine/hydroxychloroquine.
Guttate psoriasis can turn into plaque psoriasis, but it can also heal completely. Topically applied corticosteroids are used in adults often in combination with UVB light therapy and, if necessary, additional treatment of the triggering disease. In children, light therapy should be used with restraint.
Psoriatic Erythroderma
In psoriatic erythroderma, the entire skin is diseased. The skin is completely reddened with inflammation and usually shows a rather fine, loose scaling. Erythroderma is the most severe form of plaque psoriasis and the rarest. There is often severe itching.
Patients feel very ill, have a fever, are fatigued, complain of weight loss and painful joints. The lymph nodes are swollen. Psoriatic erythroderma is usually treated as an inpatient in a skin clinic. Internal medications are always used along with external therapy.
Pustular Psoriasis (psoriasis pustulosa)
In this form, spots (areas) with pustules appear on the skin. The pustules contain mainly white blood cells (neutrophilic granulocytes). While pustules are often caused by infection with bacteria, the contents of psoriatic pustules are sterile. They do not contain bacteria. The pustules are about three millimeters in size and yellowish in color. They burst after some time and dry up, leaving a yellowish crust. Sometimes these pustules appear around foci of plaque psoriasis. The pustules appear very suddenly and especially in the peripheral area of the foci. Often the pustules "grow together" to form a "pustule blanket".
Pustular forms of psoriasis are linked to triggers. It is often preceded by inflammation of the tonsils (streptococcal infection). The use of drugs with active ingredients such as lithium, beta-blockers, ACE inhibitors, chloroquine/hydroxychloroquine are also considered typical triggers. Pustular psoriasis is almost always treated internally. The most important agents are retinoids, methotrexate (MTX) or ciclosporin.
PUVA light therapy may also be useful. Biologics and their biosimilars from the group of tumor necrosis factor antagonists (adalimumab, certolizumab, etanercept, infliximab) as well as the interleukin 17 inhibitors can also be used.
Pustules on the Hands and Feet (pustulosis palmoplantaris (PPP))
Today, this form is no longer attributed to psoriasis; it is considered an independent clinical picture. PPP is restricted exclusively to the palms of the hands and/or soles of the feet. On reddened skin are skin pustules, which in very severe disease can coalesce into small pus lakes. Fresh yellowish pustules and older brown pustules with dried contents and often small annular scaly ruffles are found side by side. If the area is large and there are many fresh yellow pustules, the disease is painful and significantly restricts walking or reaching.
The relapse rate of the disease is remarkably high. It has been scientifically proven that smoking can worsen the course of the disease and increase the relapse rate. Small individual foci can be treated well with externally applied, highly effective corticosteroids. In moderately severe disease, external administration of corticosteroids is supplemented by bath or cream PUVA light therapy. In severe cases, internal medications are given.
Generalized Pustular Psoriasis (GPP)
An independent form of pustular disease is pustular psoriasis distributed over the entire body (generalized pustular psoriasis or pustular psoriasis generalisata). This form, like psoriatic erythroderma, is one of the most severe psoriatic diseases. Many pustules appear very quickly, within hours, on inflammatory reddened skin. The pustules are distributed over a large area of the whole body (generalized). Many patients with generalized pustular psoriasis did not previously have plaque psoriasis as an underlying disease. The general condition of patients with the disease is usually severely impaired, they have a fever and feel fatigued. Treatment must be conducted as an inpatient in a skin clinic. Often, internal measures are also necessary. The therapy is a combination of internal and external medication. External treatment is only supportive, because GPP must usually be treated with internal medication.
In the pustular forms of psoriasis, dithranol should not be used externally and attention must also be paid to the maximum treatable body surface area with the other active ingredients (corticoids, vitamin D3 analogues).
The first drug developed for GPP is spesolimab, which is available for severe cases. Since it is not yet commercially available, it is currently only dispensed through specialized skin clinics.
Paradoxical Psoriasis
With a growing understanding of the underlying inflammation in psoriasis, it is now well established that psoriasis shares some similarity with chronic enteric diseases (CED) and rheumatoid arthritis in the inflammatory mediators involved.
For this reason, patients with rheumatism or IBD are sometimes treated with the same biologics or biosimilars as those with psoriasis. In a few of these treated people with rheumatism or CED, a so-called paradoxical psoriasis occurs in this context. This is called paradoxical because the biologic can also improve psoriasis.
In individual cases, however, the drug used for the treatment of rheumatism can also trigger psoriasis. In this form of psoriasis, the head, hands and feet are often more affected. These areas of the body can be treated well in most cases. If the underlying therapy must be changed, psoriasis usually heals on its own.
Psoriatic Arthritis
The term refers to an inflammatory disease of the joints that occurs in addition in about 20 percent of patients with psoriasis of the skin. In most patients (over 80 percent), there is initially only psoriasis of the skin for many years before psoriatic arthritis is added. Although a certain pattern of the disease suggests psoriatic arthritis, in most cases the diagnosis is only made when typical skin and nail changes are present at the same time and the so-called rheumatoid factor is absent. This factor can typically be detected in the blood of patients with rheumatoid arthritis.
In the few sufferers who develop psoriatic arthritis before (about 10 percent) psoriasis of the skin or even without skin symptoms (less than 10 percent), diagnosis can be difficult.
Psoriatic arthritis is twice as common in patients with nail involvement as in those without. Close examination of the entire skin, including the navel, anal crease and hairy head, is important to identify previously undetected individual, sometimes very small psoriatic foci.
A special feature of psoriatic arthritis compared to other rheumatic diseases is its clinical diversity. Psoriatic arthritis can manifest itself as inflammation of the synovium (synovitis), the bones (osteitis and osteomyelitis) and the periosteum (periostitis), as well as the attachment of joint capsules, tendons or ligaments close to the joint (enthesitis). Different patterns of the disease can be distinguished. These include inflammation of the small joints of the fingers and/or toes. Involvement of all joints of a finger (disease in the beam) or inflammation of only the terminal joints in the fingertips (DIP arthritis) are typical.
Frequently, inflammatory swelling of the finger tendons (dactylitis) changes to a thickened finger or toe. With pronounced psoriatic arthritis, many small joints are diseased. In addition, individual large joints, for example the knee joints, can become diseased (oligoarthritis).
Bony destruction of the joints (arthritis mutilans) occurs in about five percent of those affected. About 40 percent of patients with psoriatic arthritis have back pain or pain in the coccyx joints because of spinal involvement.
Psoriatic arthritis may present with morning stiffness associated with a start-up pain that improves with exercise.
In case of disease of the axial skeleton and sacroiliac joint (sacroiliac joint), in addition to nocturnal pain in the back, pain in the buttocks and restriction of movements of the head may occur. Inflammation of the tendons (enthesitis) may manifest as spontaneous pain or pressure pain. Swelling close to the joint and pain limit mobility. It is common for inflammation of the tendons to progress without any clear symptoms and to go unnoticed by those affected.
In psoriatic arthritis, the attachment of the Achilles tendon to the heel and the tendon plate of the sole of the foot attached to the heel bone are more frequently diseased. Also, around the spine and at the joints around the upper ribs, the breastbone and the collarbone, inflammations of the tendons can occur quite frequently.
When selecting an appropriate therapy, the extent, course, impairment, response, and tolerability of previous therapies should be considered. In patients with skin and joint disease, therapy should target inflammation in the skin and joints.
In mild psoriatic arthritis without skin involvement, azulfidines or non-steriodal anti-rheumatic drugs (NSAIDs) may help. Leflunomide can also be used alone or in combination with MTX for predominantly joint involvement. Accompanying this, physiotherapeutic measures and orthopedic aids may be useful if inflammation and pain are controlled. Injections with cortisone should be considered for disease of individual larger joints.
However, none of the therapies are suitable for treating the skin symptoms of psoriasis.
Methotrexate (MTX) has been used for many years as a basic antirheumatic therapy with a favorable effect also on the skin. However, MTX often has only a moderate and delayed effect on more severe skin symptoms. High-quality studies demonstrating the efficacy of MTX in psoriatic arthritis are not available.
The biologicals and biosimilars approved for the treatment of psoriatic arthritis are significantly more effective than all the therapies used to date. They are prescribed when other measures do not show sufficient efficacy, have no prospect of being sufficiently effective, or cannot be given. Biologicals and biosimilars from the group of TNF-α inhibitors and interleukin-17 as well as interleukin-23 inhibitors show good efficacy against several forms of psoriatic arthritis, including inflammation of the tendons and finger joints (enthesitis/dactylitis). They also work very well against skin inflammations.
The advantage of these drugs is also the prevention of progression of psoriatic arthritis. There may even be a slight improvement of existing destruction of bones.
Psoriatic Arthritis
The term refers to an inflammatory disease of the joints that occurs in addition in about 20 percent of patients with psoriasis of the skin. In most patients (over 80 percent), there is initially only psoriasis of the skin for many years before psoriatic arthritis is added. Although a certain pattern of the disease suggests psoriatic arthritis, in most cases the diagnosis is only made when typical skin and nail changes are present at the same time and the so-called rheumatoid factor is absent. This factor can typically be detected in the blood of patients with rheumatoid arthritis.
In the few sufferers who develop psoriatic arthritis before (about 10 percent) psoriasis of the skin or even without skin symptoms (less than 10 percent), diagnosis can be difficult.
Psoriatic arthritis is twice as common in patients with nail involvement as in those without. Close examination of the entire skin, including the navel, anal crease and hairy head, is important to identify previously undetected individual, sometimes very small psoriatic foci.
A special feature of psoriatic arthritis compared to other rheumatic diseases is its clinical diversity. Psoriatic arthritis can manifest itself as inflammation of the synovium (synovitis), the bones (osteitis and osteomyelitis) and the periosteum (periostitis), as well as the attachment of joint capsules, tendons or ligaments close to the joint (enthesitis). Different patterns of the disease can be distinguished. These include inflammation of the small joints of the fingers and/or toes. Involvement of all joints of a finger (disease in the beam) or inflammation of only the terminal joints in the fingertips (DIP arthritis) are typical.
Frequently, inflammatory swelling of the finger tendons (dactylitis) changes to a thickened finger or toe. With pronounced psoriatic arthritis, many small joints are diseased. In addition, individual large joints, for example the knee joints, can become diseased (oligoarthritis).
Bony destruction of the joints (arthritis mutilans) occurs in about five percent of those affected. About 40 percent of patients with psoriatic arthritis have back pain or pain in the coccyx joints because of spinal involvement.
Psoriatic arthritis may present with morning stiffness associated with a start-up pain that improves with exercise.
In case of disease of the axial skeleton and sacroiliac joint (sacroiliac joint), in addition to nocturnal pain in the back, pain in the buttocks and restriction of movements of the head may occur. Inflammation of the tendons (enthesitis) may manifest as spontaneous pain or pressure pain. Swelling close to the joint and pain limit mobility. It is common for inflammation of the tendons to progress without any clear symptoms and to go unnoticed by those affected.
In psoriatic arthritis, the attachment of the Achilles tendon to the heel and the tendon plate of the sole of the foot attached to the heel bone are more frequently diseased. Also, around the spine and at the joints around the upper ribs, the breastbone and the collarbone, inflammations of the tendons can occur quite frequently.
When selecting an appropriate therapy, the extent, course, impairment, response, and tolerability of previous therapies should be considered. In patients with skin and joint disease, therapy should target inflammation in the skin and joints.
In mild psoriatic arthritis without skin involvement, azulfidines or non-steriodal anti-rheumatic drugs (NSAIDs) may help. Leflunomide can also be used alone or in combination with MTX for predominantly joint involvement. Accompanying this, physiotherapeutic measures and orthopedic aids may be useful if inflammation and pain are controlled. Injections with cortisone should be considered for disease of individual larger joints.
However, none of the therapies are suitable for treating the skin symptoms of psoriasis.
Methotrexate (MTX) has been used for many years as a basic antirheumatic therapy with a favorable effect also on the skin. However, MTX often has only a moderate and delayed effect on more severe skin symptoms. High-quality studies demonstrating the efficacy of MTX in psoriatic arthritis are not available.
The biologicals and biosimilars approved for the treatment of psoriatic arthritis are significantly more effective than all the therapies used to date. They are prescribed when other measures do not show sufficient efficacy, have no prospect of being sufficiently effective, or cannot be given. Biologicals and biosimilars from the group of TNF-α inhibitors and interleukin-17 as well as interleukin-23 inhibitors show good efficacy against several forms of psoriatic arthritis, including inflammation of the tendons and finger joints (enthesitis/dactylitis). They also work very well against skin inflammations.
The advantage of these drugs is also the prevention of progression of psoriatic arthritis. There may even be a slight improvement of existing destruction of bones.
Psoriasis in Children
Psoriasis affects approximately 50 percent of all patients before the age of 18. An S2 guideline has been published for this age group (Eisele 2021).
Childhood psoriasis (juvenile psoriasis) has a number of special features, both in appearance and in therapy. Approximately 0.7 to 1.0 percent of all children and adolescents develop psoriasis. It is frequently associated with bacterial (pharyngitis/neck inflammation) or even viral infections of the upper respiratory tract. Spontaneous healing is slightly more common than in adults and occurs in approximately 35 percent of children.
Childhood psoriasis often starts very suddenly and initially often also appears on the face (in about 40 percent of children). The foci on the arms, legs, chest and back are clearly reddened, but usually only scaled lightly. Salicylic acid should not be used in infants and young children. Deaths have occurred in infants from salicylic acid.
Basic therapy with skin care products as well as external treatment with corticosteroids are in the foreground. Calcipotriol in ointment base may be used from the age of six. Furthermore, dithranol (cignolin, anthralin) in ointments is available, but requires intensive co-care by the physician. UV light therapy is used with restraint in children, but internal treatment in severe cases is indicated. Five biologicals are currently approved for this purpose in children (see Table 1, page 19).
Psoriasis in Children
Psoriasis affects approximately 50 percent of all patients before the age of 18. An S2 guideline has been published for this age group (Eisele 2021).
Childhood psoriasis (juvenile psoriasis) has a number of special features, both in appearance and in therapy. Approximately 0.7 to 1.0 percent of all children and adolescents develop psoriasis. It is frequently associated with bacterial (pharyngitis/neck inflammation) or even viral infections of the upper respiratory tract. Spontaneous healing is slightly more common than in adults and occurs in approximately 35 percent of children.
Childhood psoriasis often starts very suddenly and initially often also appears on the face (in about 40 percent of children). The foci on the arms, legs, chest and back are clearly reddened, but usually only scaled lightly. Salicylic acid should not be used in infants and young children. Deaths have occurred in infants from salicylic acid.
Basic therapy with skin care products as well as external treatment with corticosteroids are in the foreground. Calcipotriol in ointment base may be used from the age of six. Furthermore, dithranol (cignolin, anthralin) in ointments is available, but requires intensive co-care by the physician. UV light therapy is used with restraint in children, but internal treatment in severe cases is indicated. Five biologicals are currently approved for this purpose in children (see Table 1, page 19).
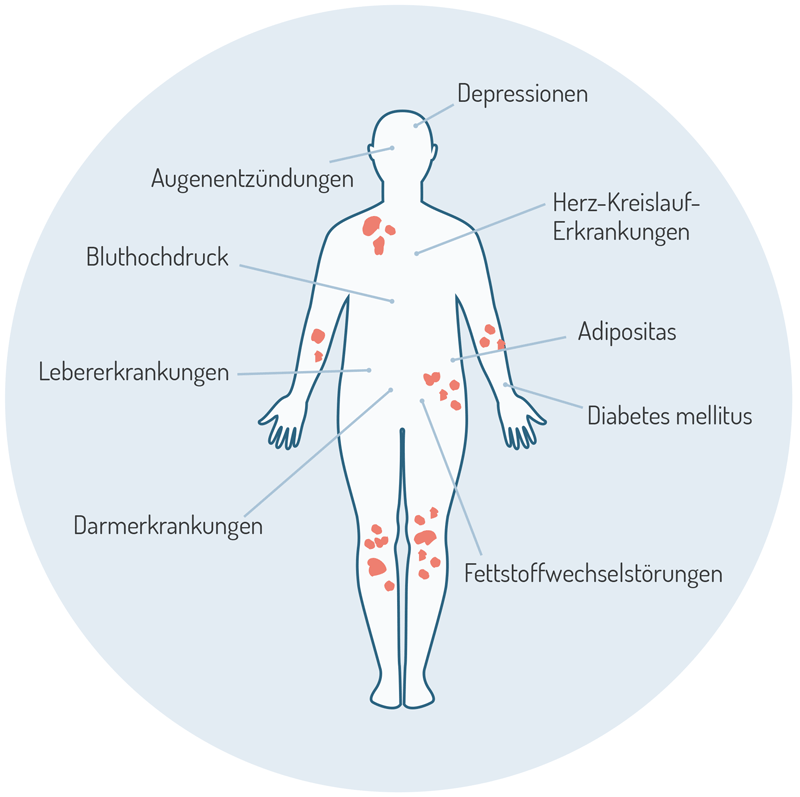
Concomitant Diseases
In the decision-making process of psoriasis therapy, not only the subjective complaints and the symptoms on the skin are considered, but also pre-existing and concomitant diseases, concomitant medication and other risk factors. Of particular importance is the presence of concomitant diseases, some of which are significantly more common in psoriasis. These include, above all, cardiovascular diseases (arteriosclerosis, circulatory disorders, coronary heart disease, myocardial infarction, stroke), metabolic diseases such as diabetes mellitus, lipid metabolism disorders, depression and anxiety disorders, as well as a variety of other chronic inflammatory diseases (rheumatic diseases, chronic inflammatory bowel diseases). Of importance, for example, is the co-inflammation of the vascular walls, which can lead to arterial disease, as well as inflammation in adipose tissue, which itself can produce inflammatory messengers and thus exacerbate other inflammatory diseases.
Basically, the inflammation of psoriasis today is therefore not regarded as pure skin inflammation, but as an inflammation of other tissues as well, so that one speaks of "systemic inflammation". The tendency to systemic inflammation is genetically co-determined, but is exacerbated by lifestyle factors such as overeating, smoking and lack of exercise. Severe skin involvement is therefore associated with a higher risk of severe other inflammatory diseases. Due to comorbidity, untreated psoriasis leads to a reduction in life expectancy by several years. Conversely, modern system therapy can reduce this mortality according to the latest data.
Comorbidity is important for several reasons: On the one hand, the diseases can represent risk factors for the therapy of psoriasis and worsen during therapy. For example, MTX and fumaric acid esters should not be used in the presence of severe liver or kidney disease, respectively, and TNF-α inhibitors should not be used in the presence of preceding malignant tumors. Second, the goal should be to treat comorbidity as well. In this context, it may be necessary to plan a targeted therapy with other specialties. Sometimes, however, comorbidity can be treated together with the psoriasis therapy, for example in the case of an autoimmune disease of the intestine or arthritis.
An important measure in the care of psoriasis is therefore the early detection of comorbidity. For this reason, German dermatologists, together with many other specialties, have issued a recommendation paper for the early detection of comorbidity, which should be a binding standard. To better achieve this, the representatives of the regional psoriasis networks (PsoNet) have also declared the early detection of psoriatic arthritis and of psoriasis comorbidity as important goals in their National Care Targets.
Concomitant Diseases
In the decision-making process of psoriasis therapy, not only the subjective complaints and the symptoms on the skin are considered, but also pre-existing and concomitant diseases, concomitant medication and other risk factors. Of particular importance is the presence of concomitant diseases, some of which are significantly more common in psoriasis. These include, above all, cardiovascular diseases (arteriosclerosis, circulatory disorders, coronary heart disease, myocardial infarction, stroke), metabolic diseases such as diabetes mellitus, lipid metabolism disorders, depression and anxiety disorders, as well as a variety of other chronic inflammatory diseases (rheumatic diseases, chronic inflammatory bowel diseases). Of importance, for example, is the co-inflammation of the vascular walls, which can lead to arterial disease, as well as inflammation in adipose tissue, which itself can produce inflammatory messengers and thus exacerbate other inflammatory diseases.
Basically, the inflammation of psoriasis today is therefore not regarded as pure skin inflammation, but as an inflammation of other tissues as well, so that one speaks of "systemic inflammation". The tendency to systemic inflammation is genetically co-determined, but is exacerbated by lifestyle factors such as overeating, smoking and lack of exercise. Severe skin involvement is therefore associated with a higher risk of severe other inflammatory diseases. Due to comorbidity, untreated psoriasis leads to a reduction in life expectancy by several years. Conversely, modern system therapy can reduce this mortality according to the latest data.
Comorbidity is important for several reasons: On the one hand, the diseases can represent risk factors for the therapy of psoriasis and worsen during therapy. For example, MTX and fumaric acid esters should not be used in the presence of severe liver or kidney disease, respectively, and TNF-α inhibitors should not be used in the presence of preceding malignant tumors. Second, the goal should be to treat comorbidity as well. In this context, it may be necessary to plan a targeted therapy with other specialties. Sometimes, however, comorbidity can be treated together with the psoriasis therapy, for example in the case of an autoimmune disease of the intestine or arthritis.
An important measure in the care of psoriasis is therefore the early detection of comorbidity. For this reason, German dermatologists, together with many other specialties, have issued a recommendation paper for the early detection of comorbidity, which should be a binding standard. To better achieve this, the representatives of the regional psoriasis networks (PsoNet) have also declared the early detection of psoriatic arthritis and of psoriasis comorbidity as important goals in their National Care Targets.
The DPB promotes exchange between those affected through regional self-help groups, which offer valuable support and information. These groups allow to share experiences, encourage each other and find ways to deal with the disease together. Further information can be found on the DPB website under regional groups [German].
The DPB promotes exchange between those affected through regional self-help groups, which offer valuable support and information. These groups allow to share experiences, encourage each other and find ways to deal with the disease together. Further information can be found on the DPB website under regional groups [German].
The DPB offers topic-specific online groups for anyone who would like to exchange ideas regardless of location. These groups allow to share experiences and support each other. If necessary, medical experts can be brought in to answer participants' questions. Further information on the online groups can be found on the DPB website [German].
The DPB offers topic-specific online groups for anyone who would like to exchange ideas regardless of location. These groups allow to share experiences and support each other. If necessary, medical experts can be brought in to answer participants' questions. Further information on the online groups can be found on the DPB website [German].
The DPB offers many brochures and guides that provide comprehensive information and practical tips on living with psoriasis. These materials cover topics such as self-management, treatment options and legal aspects and are available to both members and interested parties. You can find an overview of the available publications on the DPB website [German].
The DPB offers many brochures and guides that provide comprehensive information and practical tips on living with psoriasis. These materials cover topics such as self-management, treatment options and legal aspects and are available to both members and interested parties. You can find an overview of the available publications on the DPB website [German].
For individual medical care, it can be helpful to consult specialists. The DPB offers a directory of specialists to help members find experienced dermatologists or other specialists. Further information can be found on the DPB website [German].
For individual medical care, it can be helpful to consult specialists. The DPB offers a directory of specialists to help members find experienced dermatologists or other specialists. Further information can be found on the DPB website [German].
An annual membership fee of €59 (reduced rate €39) not only gives you access to the directory of medical specialists, but also to many other benefits such as free medical or legal advice and six issues of PSO Magazine every year. Together you are less alone - and better informed!
An annual membership fee of €59 (reduced rate €39) not only gives you access to the directory of medical specialists, but also to many other benefits such as free medical or legal advice and six issues of PSO Magazine every year. Together you are less alone - and better informed!
This website was kindly supported financially by the companies mentioned below.